
Why climate change is a global health issue
We explore the future impact of the global climate crisis on peoples' health and health systems, and why framing it in this way might be useful.

- Climate Change | COP26
From 31 October – 12 November 2021, the countries of the United Nations are reconvening in Glasgow for the 26th annual climate change summit, dubbed COP26. This takes place against the backdrop of a year blighted by unusual and extreme weather patterns and a world recovering and still muddling through the effects of the COVID19 pandemic.
Here, we take a look at how climate change is a health issue that has the potential for far-reaching knock-on effects on our global healthcare providers, systems, and emergency services. We’ll also explore how healthcare providers can be at the forefront of leading on climate action and the potential benefits of framing the climate crisis as a health issue.
Climate change is a broad and far-reaching issue with the potential to disrupt all aspects of society. How it impacts different communities and demographics is complex, making it one of the hardest issues modern days to tackle, particularly as a collective.
The Paris Agreement, largely cited as the key underpinning legislation of governmental climate action was established in 2016 following COP21. Crucially, it highlights that climate change is not only a concern for humankind and human rights but that the ‘right to health’ was a key human right to be considered in the fight against climate change.
Healthcare, as both a service and industry, forms part of the social, economic and political landscape of a country. The emerging issues around climate change could, directly and indirectly, undermine decades of human progress made by the medical and healthcare community. As the effects of the COVID19 pandemic goes to show, the stability of healthcare infrastructure is crucial to protect the global population.
Climate change as a health issue
Climate change will change how we consider and care for our health — individually, and as societies. Its effects are both direct — physiological effects such as worsening air quality leading to an increase in respiratory issues — and indirect — for example, ecological changes disrupting food chains and threatening safe water supplies. Some examples of health concerns include, but are not limited to:
- Injury or death due to extreme weather events
- Worsening air quality increasing the prevalence and severity of respiratory issues
- Disruption to food chain supplies resulting in hunger and malnutrition
- Rising sea levels threatening freshwater supplies and safe drinking water and
- Disease transmission in crowded populations that lack sanitary infrastructures.
With a growing and aging global population, the demands on our global healthcare infrastructures will inevitably increase in other ways too.

Implications of climate change for healthcare systems and services
In the future, healthcare systems will need to evolve to manage the impact of climate-sensitive health issues and extreme weather.
During extreme weather events, such as heatwaves, cold snaps, and flooding, ambulance call-outs can increase by 25 – 35%. Emergency services operating in these circumstances may need to navigate power outages, access issues, and more.
As well as the increased demand that healthcare services are likely to deal with due to single events, there will also be a need for more long-term resource management and resilience due to the health implications of climate change. This includes diseases and conditions that take more time to become symptomatic and require treatment, such as respiratory problems caused by air pollution.
The above are examples of direct impacts, but there are also indirect implications to health services that result from climate change. An example of this is extreme weather such as hurricanes and flooding threatening the stability of the supply chains that serve the healthcare industry.
When Hurricane Maria made landfall in 2017 in Puerto Rico, a major global pharmaceutical company reported having lost an estimated $175 million worth of stock. It took the country weeks to restore communication networks and many displaced workers relied on temporary shelters powered by diesel generators until power was restored.
There is a long-standing need for healthcare systems to progress towards climate-resilient systems and processes, not only for their self-preservation but also that of the patients and staff that rely on them.

Healthcare leading the way
The healthcare industry is on the front line of these changes and will witness firsthand the impact climate change has. It puts them in a unique position to both present the data needed to underpin the effects of climate change and establish what safeguards they will need in the future.
Early warning systems of climate events could be established so that health facilities could prepare for extreme weather events such as storms, heatwaves and flooding and more broadly anticipate outbreaks of climate-sensitive diseases. At present, only 3% of health resources are invested in prevention, and only 0.5% of multilateral climate finance has been specifically allocated for health projects. There’s certainly a lot further to go.
The health community is highly trusted, globally-connected and increasingly engaged in reducing climate change. Following COP24 in 2018 the call to action on climate and health for COP24 was issued by organisations representing over 5 million doctors, nurses and public health professionals and 17,000 hospitals in over 120 countries.
Mobilisation of the health sector is also necessary to reduce the growing contribution of healthcare to carbon emissions, which currently represents 5 – 8% of the total across high-income countries.’.
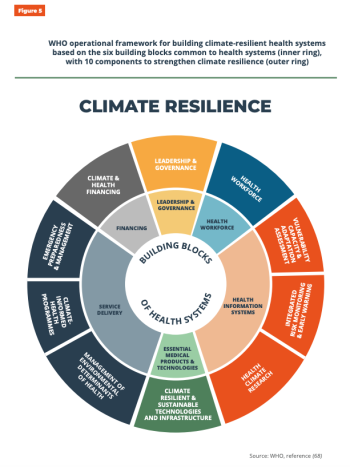
The WHO has published an operational framework for building climate-resilient health systems to help give guidance and ‘building blocks’ for healthcare systems in the future. It estimates that the value of health gains from taking appropriate and widespread climate action is about twice as large as the cost of mitigation policies.
It is by far better for healthcare providers to act now and feel the tangible benefits of reducing the risks to the population, rather than having to implement costly reactive climate change policies.
The global healthcare community is in a unique position to be an advocate for humanity and to protect our ‘right to health’, as highlighted in the Paris Agreement back in 2015.
Why framing climate change as a health issue is helpful
In the UK, as much as it dominates our topics of conversation, our weather patterns are moderately mild. Along with many countries in the global North, we feel removed from the reality of the climate crisis.
Highlighting the health implications of the climate crisis makes the issue a highly personal one. It can help people to understand the urgency of the situation and inspire them to take action and make changes on an individual level. Whilst the actions of individuals alone are not enough to combat climate change, it’s a step in the right direction and part of the wider global culture change that is needed.
One of the key issues with tackling climate change is the sheer enormity of information out there about what you should do and how to do it. The guidance is not always centralised or coming from one source of truth, so it can be overwhelming to figure out where to start.
Although much of the damage already done to the environment sadly can’t be reversed, it can be mitigated if we make it a priority — individually, nationally and globally.
Here are some great resources to get you started:
- The Climate Pledge: a cross-sector community of companies, organisations, individuals, and partners, working together to crack the climate crisis
- Make My Money Matter: ensure that your money is used sustainably by banks, pension providers, and other financial services.
- Ecologi: carbon offsetting plans for individuals, families, and businesses
- Giki Zero: free carbon footprint calculator tool
Read more about what's important to us


Launching a Virtual Stem Cell Donor Drive for Blood Cancer Awareness Month
